Catàleg general VIH

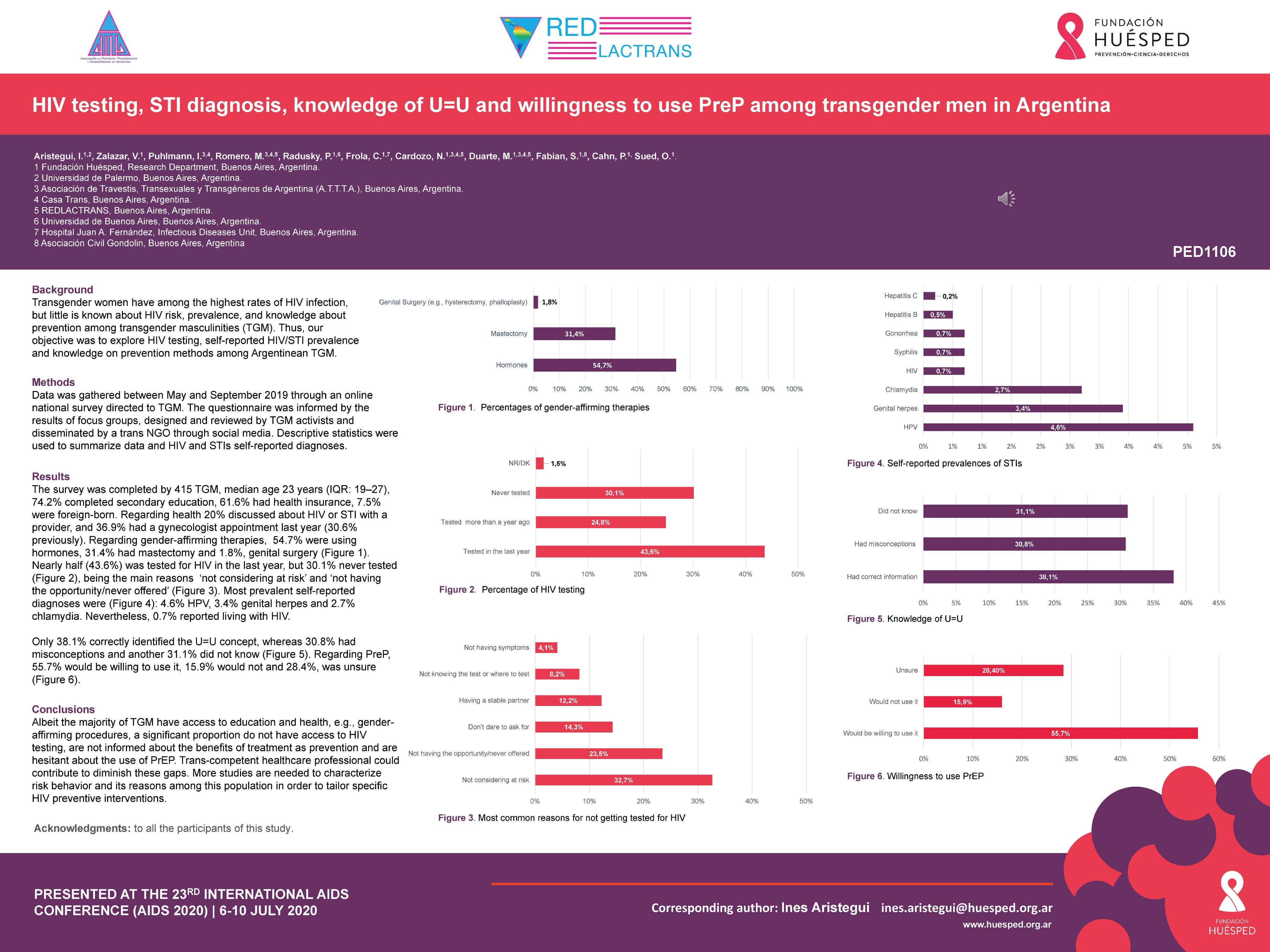
HIV testing, STI diagnosis, knowledge of U=U and willingness to use PreP among transgender men in Argentina
Resum
BACKGROUND: Transgender women have among the highest rates of HIV infection but little is known about HIV risk, prevalence, and knowledge about prevention among among transgender masculinities (TGM). Thus, our objective was to explore HIV testing, self-reported HIV/STI prevalence and knowledge on prevention methods among Argentinean TGM. METHODS: Data was gathered between May and September 2019 through an online national survey directed to TGM. The questionnaire was informed by the results of focus groups and designed and reviewed by TGM activists and disseminated by a trans NGO through social media. Descriptive statistics were used to summarize data and HIV and STIs self-reported diagnoses. RESULTS: The survey was completed by 415 TGM, median age 23 years (IQR: 19'27), 74.2% completed secondary education, 61.6% had health insurance, 7.5% were foreign-born. Regarding health 20% discussed about HIV or STI with a provider, and 36.9 had a gynecologist appointment last year (30.6 previously). Regarding gender-affirming therapies, , 54.7% were using hormones, 31.4% had mastectomy and 1.8%, genital surgery (e.g., hysterectomy, phalloplasty). Nearly half (44.2%) was tested for HIV in the last year, but 30.5% never tested, being the main reasons 'not considering at risk' (n=32), 'not having the opportunity/never offered' (n=23), 'don't dare to ask for' (n=14), 'having a stable partner' (n=12), 'not knowing the test or where to test' (n=8), 'not having symptoms' (n=4). Self-reported diagnoses were: 4.6% HPV, 3.4% genital herpes, 2.7% chlamydia, 0.7% HIV, 0.7% syphilis, 0.7% gonorrhea, 0.5% hepatitis B, 0.2% hepatitis C. Only 38.1% correctly identified the U=U concept, whereas 30% had misconceptions and another 30% did not know. Regarding PreP, 55.7% would be willing to use it, 15,9% would not and 28.4%, was unsure. CONCLUSIONS: Albeit the majority of TGM have access to education and health, e.g., gender-affirming procedures, a significant proportion do not have access to HIV testing, are not informed about the benefits of treatment as prevention and are hesitant about the use of PrEP. Trans-competent healthcare professional could contribute to diminish these gaps. More studies are needed to characterize risk behaviour and its reasons among this population in order to tailor specific HIV preventive interventions.- Tema:
Autoria:
ARISTEGUI, Inés; ZALAZAR, Virginia; PUHLMAN, I.; ROMERO, Marcela; RADUSKY, Pablo David; FROLA, Claudia E.; CARDOZO, Nadir F.; DUARTE, Mariana; FABIÁN, Solange; CAHN, Pedro; SUED, Omar
Autoria institucional: ATTTA (Asociación de Travestis, Transexuales y Transgéneros de Argentina); REDLACTRANS (Red Latinoamericana y de Caribe de Personas Trans); Fundación Huésped (Argentina)
Autoria institucional: ATTTA (Asociación de Travestis, Transexuales y Transgéneros de Argentina); REDLACTRANS (Red Latinoamericana y de Caribe de Personas Trans); Fundación Huésped (Argentina)
Fitxa bibliogràfica
- Any de publicació:
- [2020]
- Descripció física:
- [1] p.
- Format:
- Fulletó
- Tipus de document:
- Col·loquis i ponències
- Notes:
- Póster presentado en la 23rd International AIDS Conference, celebrada de manera virtual del 6 al 10 de julio de 2020.
Continguts relacionats
També et pot interessar
-
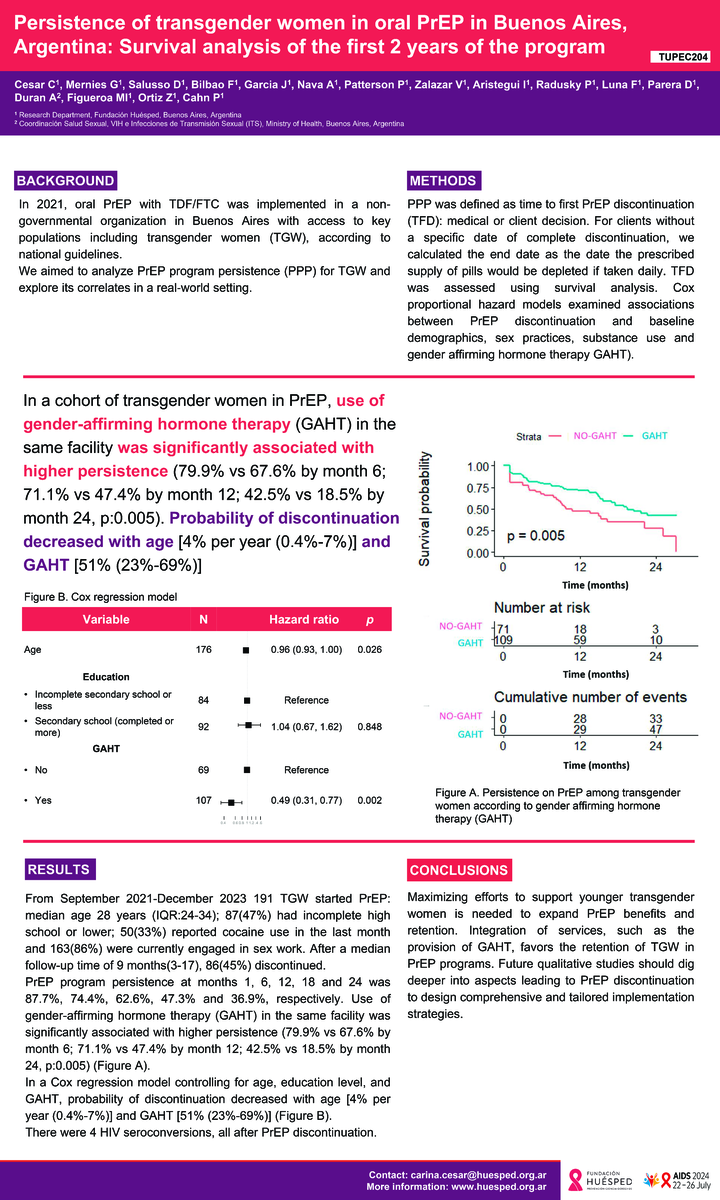
Persistence of transgender women in oral PrEP in Buenos Aires, Argentina: survival analysis of the first 2 years of the program
-
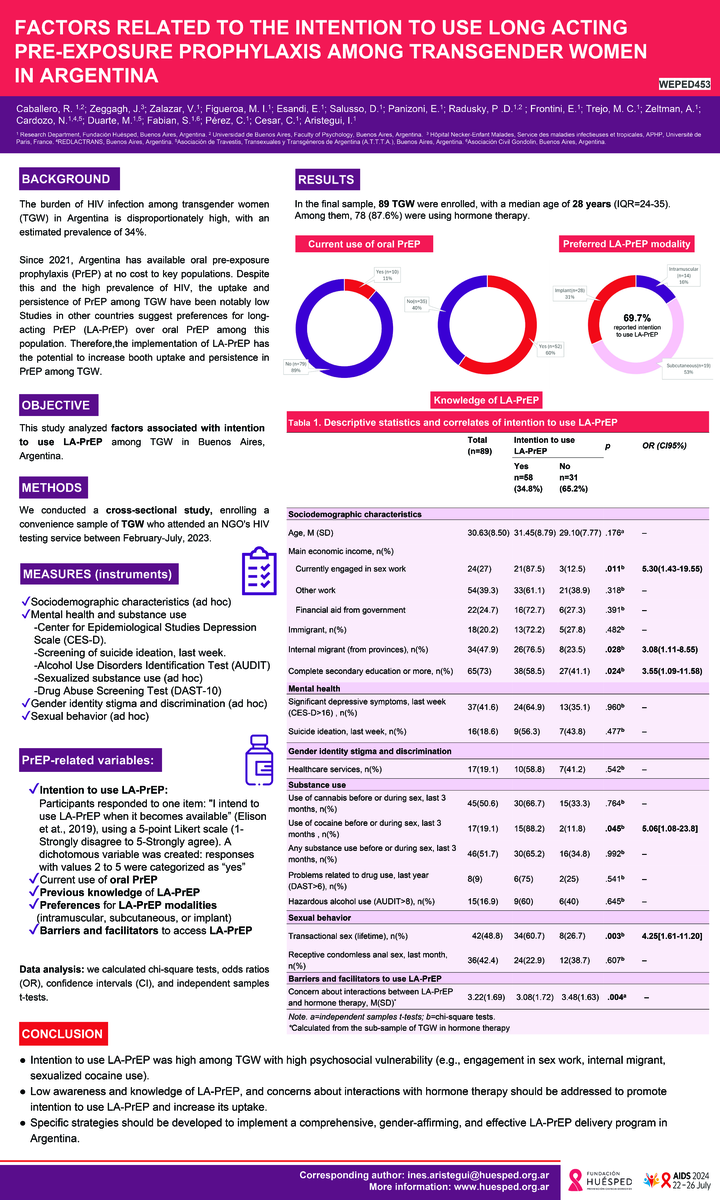
Factors related to the intention to use long acting pre-exposure among transgender women in Argentina
-
Oral PrEP persistence among key populations in a center from Buenos Aires, Argentina: survival analysis of the program's first three years