Resum
BACKGROUND: Among MSM, knowledge about the negligible risk of HIV transmission (untransmissibility) when viral load is undetectable (U=U) may lead to reduction of HIV-stigma and sexual behavior changes. The aim of this analysis is to describe the relationship between U=U knowledge and sexual behavior among MSM participating in the Latin-American Men Internet Survey (LAMIS).
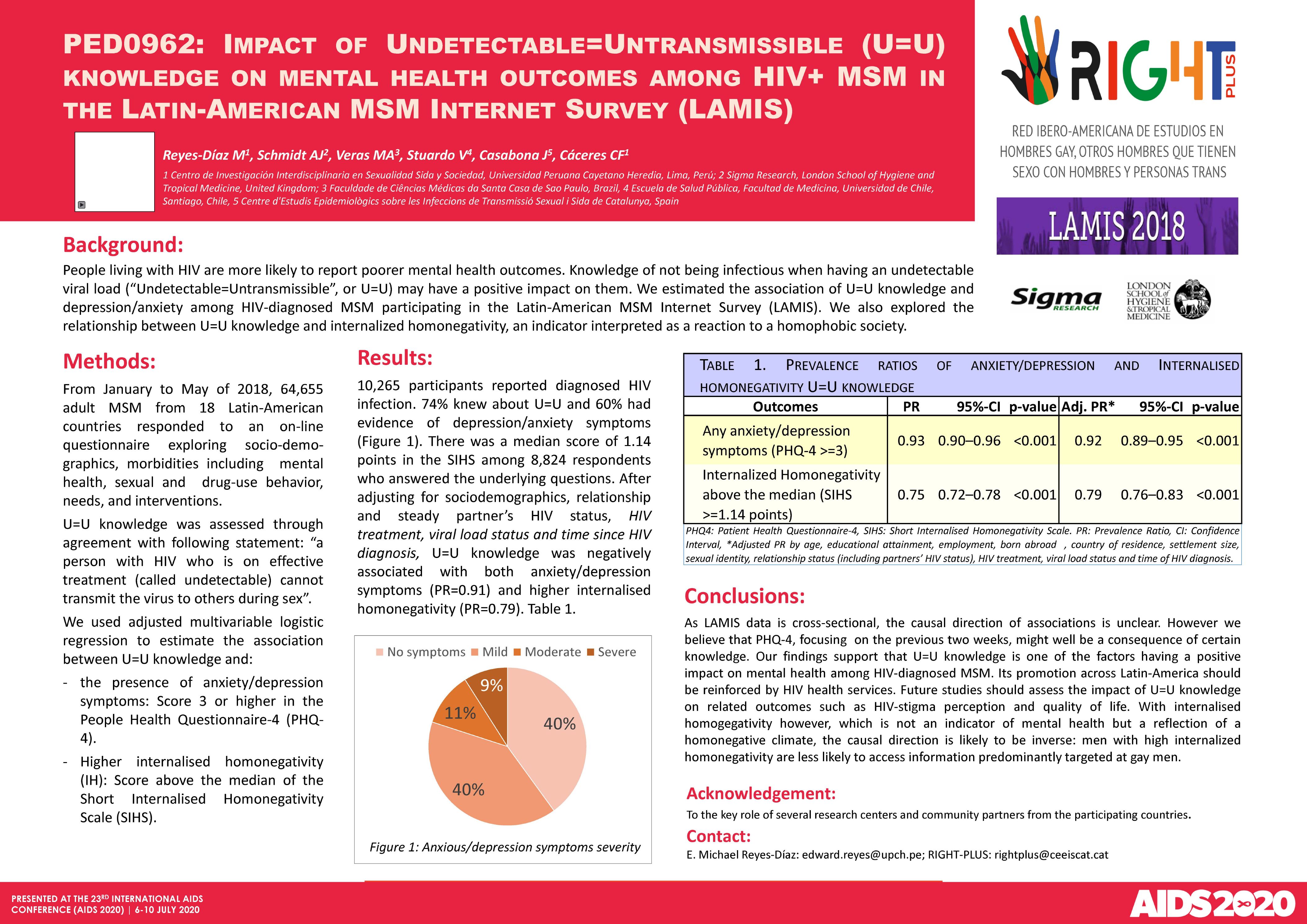
METHODS: From January to May of 2018, 64,655 adult MSM from 18 Latin-American countries responded to an online questionnaire exploring sociodemographics, mental health metrics, sexual behavior, and HIV-related knowledge and behavior. Participants reporting sex with non-steady partners in the last 12 months were included in the analysis. Stratified by self-reported HIV/viral load status, unadjusted prevalence ratios (PR) of sexual behaviors during the last sexual session with a non-steady partner (i.e. number of concurrent partners, type of venue, HIV-status communication, knowledge/assumption of partner's HIV-status, receptive/insertive condomless anal intercourse [CAI]), were assessed in relation to U=U knowledge.
RESULTS: 40,117 (83%) respondents were untested or reported their last HIV test to be negative (NEG), 6,253 (13%) reported HIV diagnosis and undetectable viral load (HIV-UVL); and 1846 (4%) reported HIV diagnosis but detectable/unknown viral load (HIV-DVL). U=U knowledge was associated with: (i) 2+ concurrent non-steady partners among NEG (PR=1.17) and HIV-UVL (PR=1.27) respondents, (ii) having sex at a sex venue among HIV-UVL respondents (PR=0.83), (iii) knowing/assuming to know a partner´s HIV-status among NEG respondents (PR=1.10), (iv) insertive CAI among HIV-UVL respondents (PR=1.15), and receptive CAI among NEG (PR=0.86) and HIV-UVL respondents (PR=1.16). No significant association was observed with communicating HIV status. CONCLUSIONS: Our preliminary findings suggest that U=U knowledge has a positive impact on HIV preventive behavior among MSM without HIV (concern about partner's HIV-status and less frequent receptive CAI) and on reducing concern about HIV transmissibility to sexual partners (more frequent CAI) among MSM with HIV but undetectable viral load.