Resumen
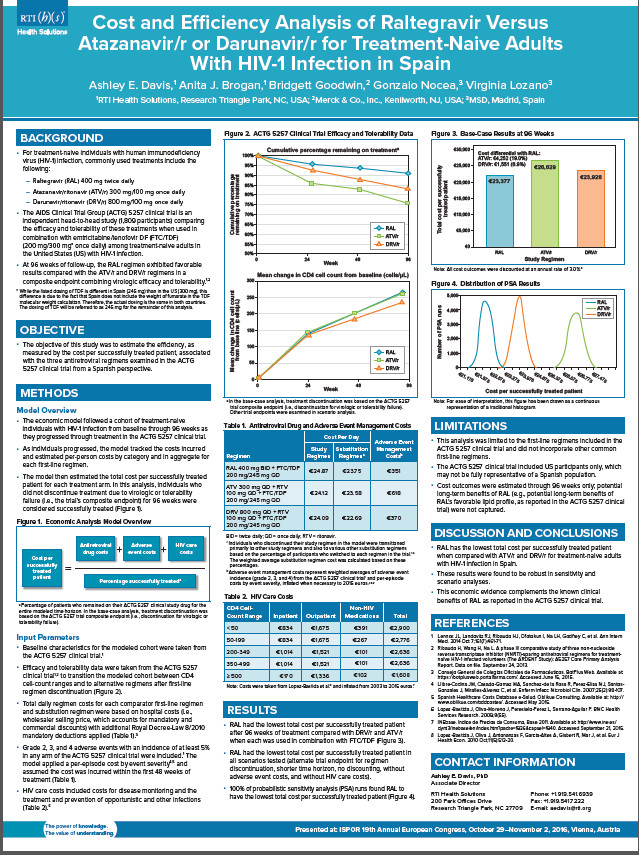
OBJECTIVES: The ACTG 5257 clinical trial showed that raltegravir (RAL) was superior to atazanavir/ritonavir (ATV/r) and darunavir/ritonavir (DRV/r), when used in combination with tenofovir DF/emtricitabine (TDF/FTC), in a 96-week composite endpoint combining virologic efficacy and tolerability for treatment-naive adults with HIV-1 infection. This study aimed to estimate costs and efficiency associated with these three regimens in Spain. METHODS: An economic model was developed to estimate costs for antiretroviral drugs, adverse event management, and HIV care for individuals initiating first-line therapy. Head-to-head efficacy and safety data (discontinuation rates based on the trial’s composite endpoint, mean CD4+ cell-count changes, adverse event incidence) up to 96 weeks for RAL, ATV/r, and DRV/r were obtained from the ACTG 5257 clinical trial. Antiretroviral drug costs were based on hospital costs with additional mandatory discounts applied. Adverse event management costs and HIV care costs, stratified by CD4+ cell-count range, were obtained from published sources and inflated to 2015 euros. Costs per successfully treated patient (i.e., remaining on first-line therapy for 96 weeks) were estimated for the three regimens and tested in sensitivity and scenario analyses. All outcomes were discounted at 3.0% per year. RESULTS: At 96 weeks, RAL was associated with higher antiretroviral drug costs, lower adverse event costs, and similar HIV care costs when compared with either ATV/r or DRV/r. Total costs per successfully treated patient were €22,377 for RAL, €26,629 for ATV/r, and €23,928 for DRV/r. These results were found to be robust in probabilistic sensitivity and scenario analyses. CONCLUSIONS: RAL has the lowest cost per successfully treated patient when compared with two other common first-line regimens, DRV/r and ATV/r, each used in combination with TDF/FTC, for treatment-naive adults with HIV-1 infection in Spain. This economic evidence further complements the known clinical benefits of RAL as reported in the ACTG 5257 clinical trial.