Resum
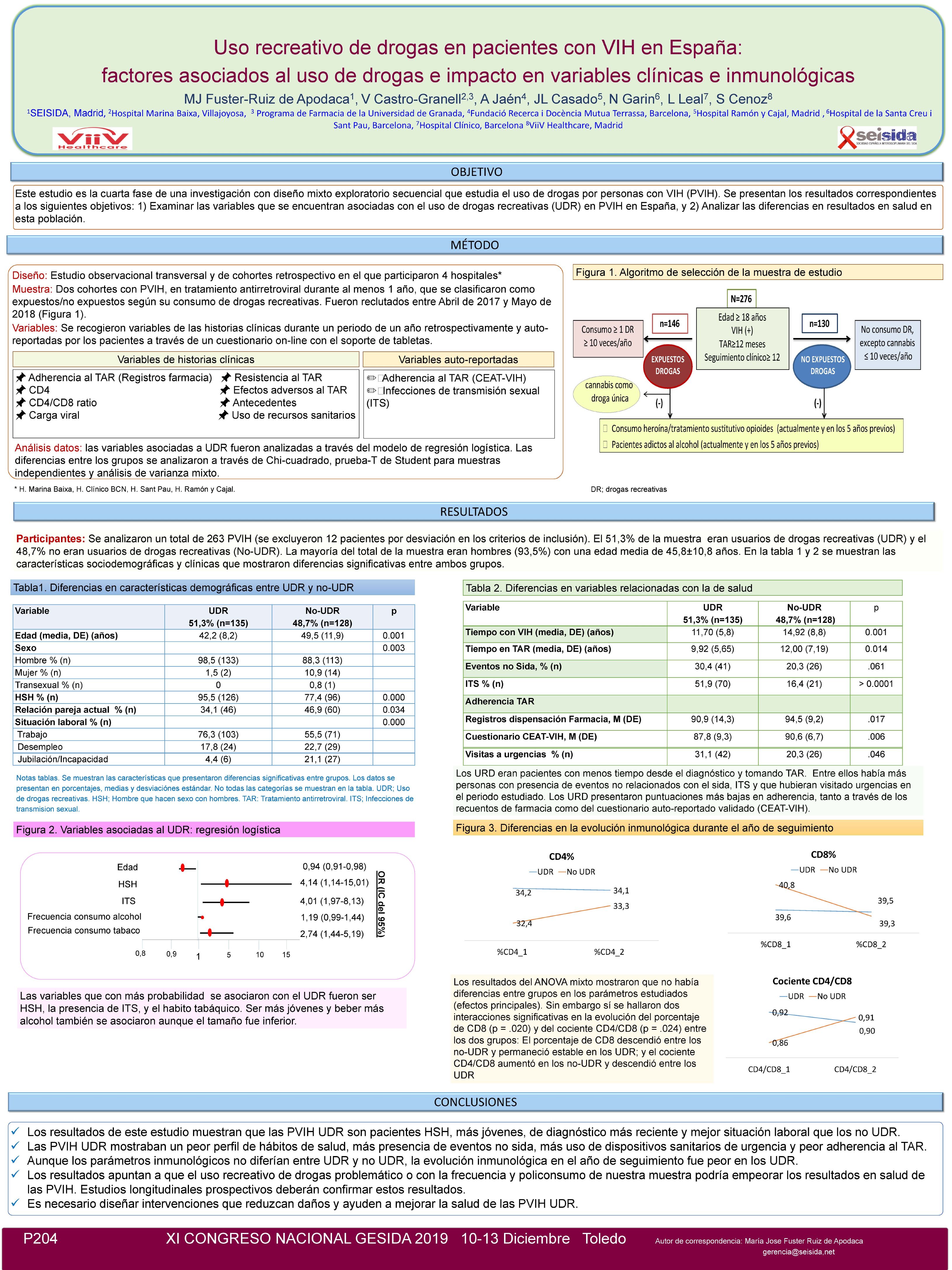
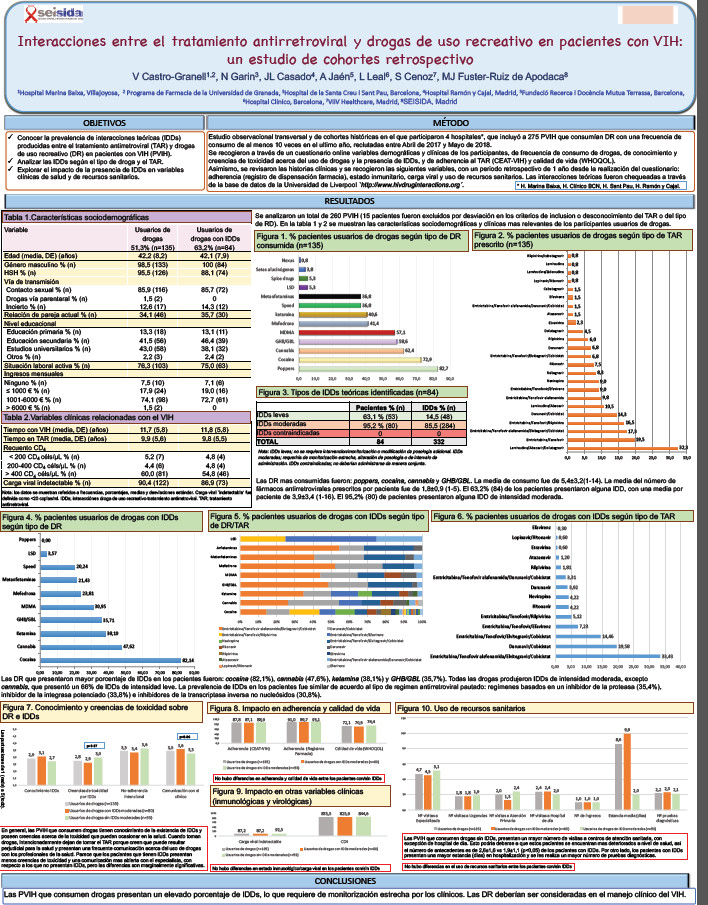
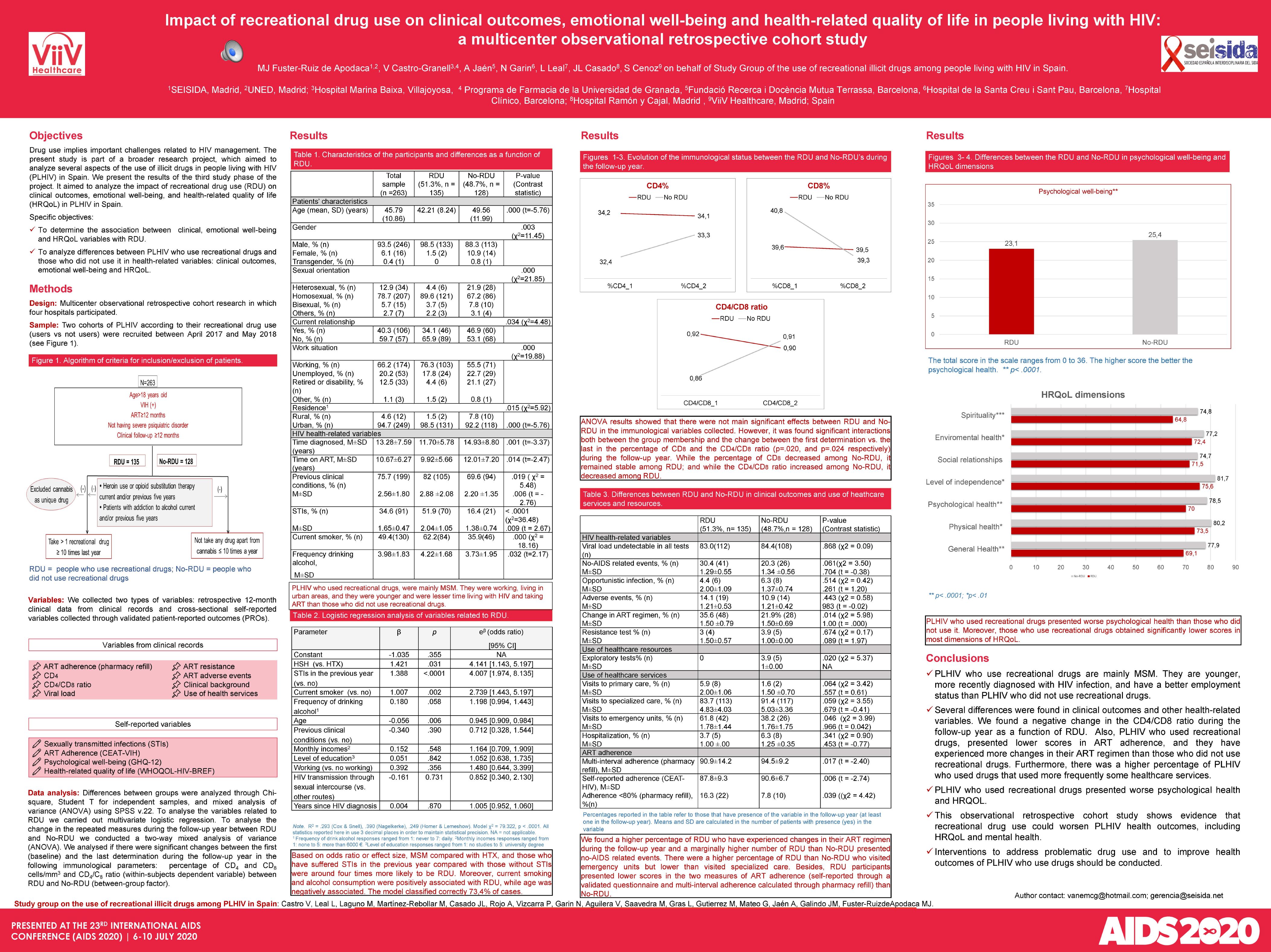
Objective: This study assessed the variables associated with recreational drug use (RDU) in people living with HIV (PLHIV) in Spain. Secondly, it examined the differences in clinical outcomes as a function of RDU in this population. Methods: Two cohorts of PLHIV taking antiretroviral therapy (ART) for at least one year were recruited between April 2017 and May 2018 according to their recreational drug use (RDU): frequent RDU (consumption =1 drug =10 times a year, excluding the use of methadone, heroin, and cannabis as a single drug) vs. non-RDU. We collected the following retrospective last 12-month clinical data from clinical records: ART adherence (pharmacy refill), CD4, CD4/CD8 ratio, viral load, resistance to and adverse effects of ART, previous clinical conditions, and use of health services. Self-reported ART adherence was measured through CEAT-VIH, and a specific question regarding sexually transmitted infections (STIs), respectively, at the inclusion visit. Variables associated with RDU were analyzed through a logistic regression model. Differences between RDU and non-RDU were analyzed through Chi-square, Student T for independent samples, and mixed analysis of variance using SPSS v.22. Results: A total of 275 PLHIV were included; 12 were excluded by protocol deviation. The final sample was composed of 51.3% RDU and 48.7% non-RDU. Most participants were male (93.5%) with an average age of 45.8±10.8 years. The variables associated with RDU were age, OR=0.94 [0.91, 0.98], men who have sex with men, OR=4.14 [1.14, 15.01], STIs, OR=4.01 [1.97, 8.13], frequency of drinking alcohol, OR=1.19 [0.99, 1.44], and smoking, OR=2.74 [1.44, 5.19]. RDU patients presented lower scores of ART adherence (p=.017, and p=.006, for multi-interval adherence and self-reported adherence respectively), more visits to emergency unit (p=.046), more non-AIDS related events (p=.061) but fewer visits to their specialist physician (p=.059), although the last two variables refer marginally significant differences. ANOVA results showed that there were non-significant main effects between RDU and non-RDU in the means of the percentage of CD4, CD8, and CD4/CD8 ratio. However, there were significant interactions both between the group membership and the change between the first determination vs. the last in the percentage of CD8 and the CD4/CD8 ratio (p=.020, and p=.024 respectively) during the follow-up year. While the percentage of CD8 decreased among non-RDU, it remained stable among RDU; and while the CD4/CD8 ratio increased among non-RDU, it decreased among RDU. Conclusions: This observational retrospective cohort study shows evidence that recreational drug use could worsen PLHIV health outcomes.