Resum
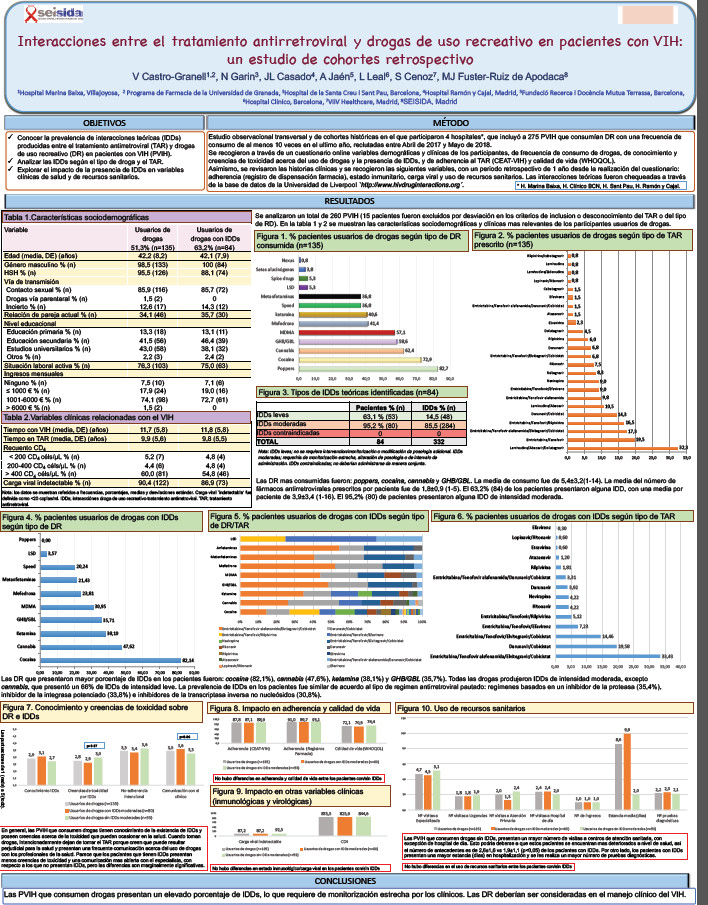
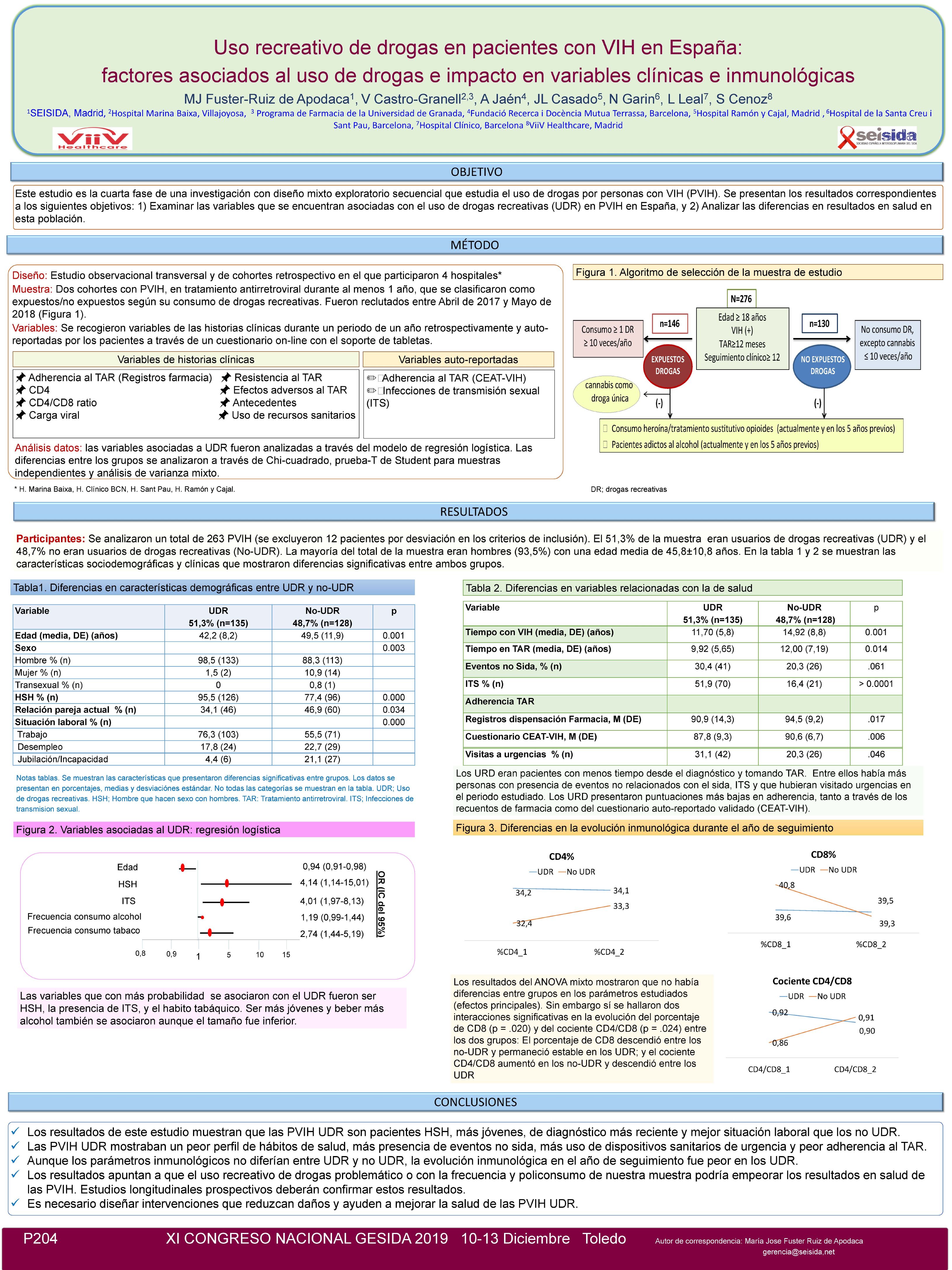
Objective: This study analyzed the prevalence and type of drug-drug interactions (DDI) between the antiretroviral therapy (ART) and recreational drugs (RDs) among people living with HIV (PLHIV) as well as their clinical impact on treatment adherence, immunological status, viral load and use of healthcare services.
Methods: A total of 275 PLHIV, recruited according to their recreational drug use (RDU), participated in a multicenter observational retrospective cohort study conducted between November 2016 and May 2017. We collected demographics, health data, drug consumption, knowledge and interaction toxicity beliefs on use of drugs and DDIs and adherence behaviors through an online survey. We compiled the following retrospective last 12-month clinical data from the clinical records: ART adherence, CD4, viral load, and use of health services. Theoretical DDIs were checked within Liverpool University database `http://www.hiv-drugnteractions.org. Results: A total of 260 PLHIV were included (15 were excluded by protocol deviation or unknown of their ART or type of RDs). Of those with RDU (n=133, 51.3%), 63.2% (n=84) presented some DDI between ART and RD, with a mean of 3.95±3.47 (1-16) DDIs per patient. Of note, potentially severe/critical DDIs were identified in 77.4% (n=65) of the patients using RDU with DDIs. The RDs most frequently involved in DDIs were cocaine (83.1%), ketamine (49.2%), GHB/GBL (46.2%), and MDMA (40.0%). DDIs prevalence was similar according to ART regimens: protease inhibitors-based regimens (35.4%), integrase inhibitors-boosted (33.8%) and non-nucleoside reverse transcriptase inhibitors (30.8%). Factors independently associated with DDIs were taking >3 different RD (OR=2.4; 95% CI: 1.1–5.7) and having >2 changes of ART during the year of follow-up [OR= 6.4; 95% CI: 1.6–24.9]. On the other hand, knowledge and beliefs on toxicity with the use of drugs and DDIs was marginally higher in those participants with DDI than in No-DDIs (3.1±1.0 vs. 2.7±1.1, p=.07). From a clinical perspective, participants with potential DDI did not present significant differences in most of the clinical variables analyzed except in the number of visits to HIV specialist, that was lower than in those without DDIs (3.96±2.69 vs. 5.55±4.78; p=.031). Conclusions: PLHIV who use drugs experience DDIs in an important proportion, requiring close monitoring. RDUs should be considered in the clinical management of HIV patients.