Resum
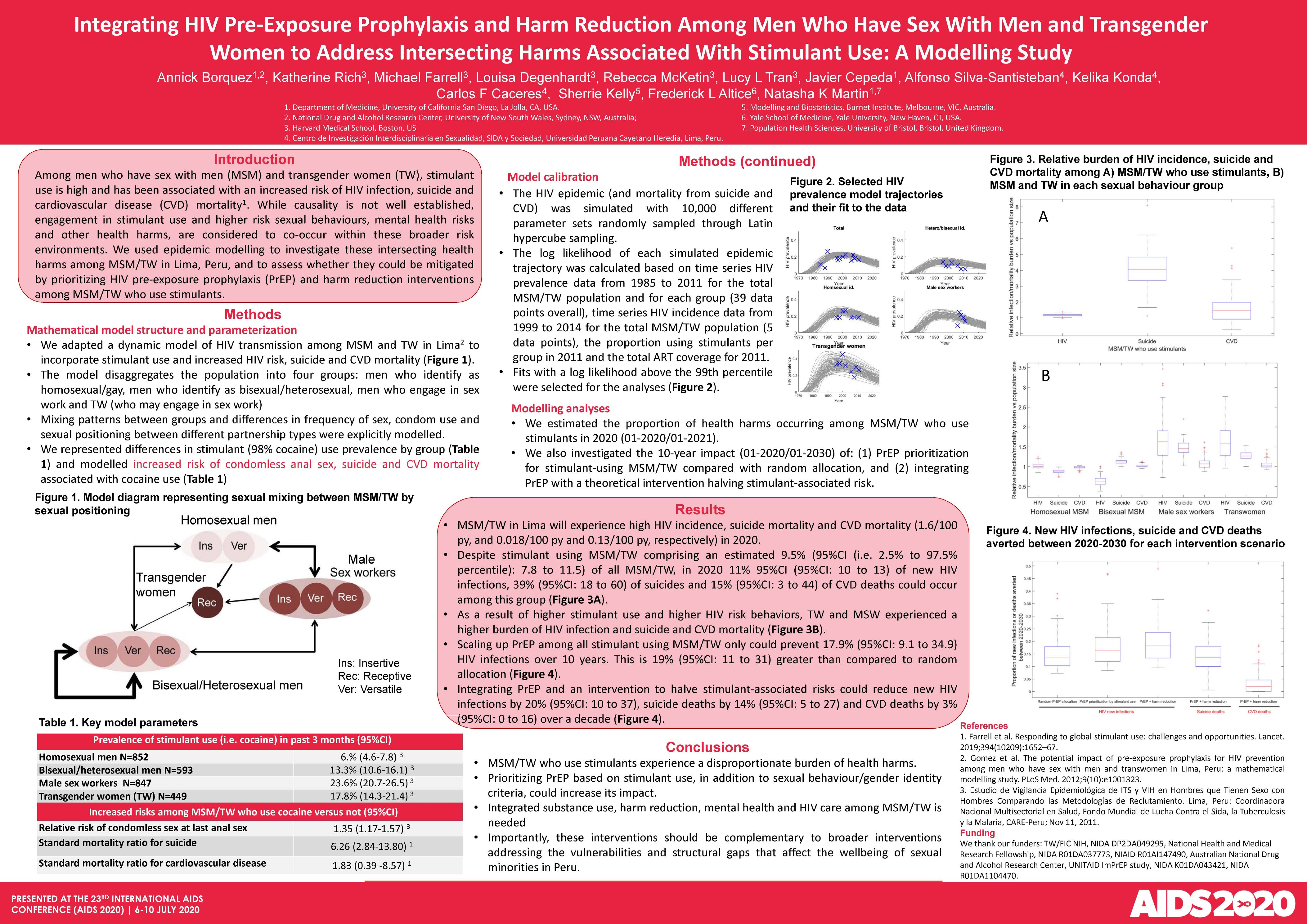
BACKGROUND: Stimulant use is often high among MSM/TW and has been associated with an increased HIV risk, suicide and CVD mortality. Quantifying the excess disease burden among MSM/TW using stimulants has important policy implications. Using epidemic modeling, we investigated these intersecting health harms among MSM/TW in Lima, Peru, and assessed the impact of prioritizing HIV pre-exposure prophylaxis (PrEP) and harm reduction interventions among MSM/TW who use stimulants. METHODS: The model represents HIV transmission, CVD and suicide mortality among MSM/TW, differentiating sexual behaviors between four main groups: homosexual and heterosexual/bisexual self-identified MSM, male sex workers and TW. We modeled the increased risk of unprotected anal sex during last encounter obtained from local data (RR=1.35 [95%CI 1.17-1.57]) and used general-population estimates from a global review to model the increased risk of suicide (SMR=6.26 [95%CI 2.84-13.80]) and CVD mortality (SMR=1.83 [95%CI: 0.39-8.57]) among MSM/TW who use stimulants. We estimated the proportion of health harms occurring among MSM/TW who use stimulants in the next year and investigated the ten-year impact (2020-2030) of PrEP prioritization for stimulant-using MSM/TW on HIV, and that of combining PrEP with harm reduction interventions that would halve stimulant use associated risks. RESULTS: Despite MSM/TW who use stimulants comprising an estimated 9.5% (95%CI: 7.8-11.5) of all MSM/TW in Lima, in the next year, 11% (2.5-97.5% Interval: 10-13%) of new HIV infections, 39% (95%I: 18-60%) of suicides and 15% (95%I: 3-44%) of CVD deaths could occur among this group. Scaling up PrEP among all MSM/TW who use stimulants would prevent 19% (95%I: 11-31%) more HIV infections across 10 years compared to random allocation. Integrating PrEP and an intervention to halve stimulant-associated risks could reduce overall new HIV infections by 20% (95%I: 10-37%), suicide deaths by 14% (95%I: 5-27%), and CVD deaths by 3% (95%I: 0-16%).
CONCLUSIONS: MSM/TW who use stimulants experience a disproportionate burden of HIV infection, suicide and CVD mortality. Prioritizing PrEP based on stimulant use, in addition to sexual behavior or gender identity criteria, could increase its impact. Importantly, as we move towards integration of HIV services, providing comprehensive substance use and mental health care could reduce health disparities among MSM/TW who use stimulants.
Autoria:
BÓRQUEZ, Annick;
RICH, Katherine;
FARRELL, Michael;
DEGENHARDT, Louisa;
MCKETIN, Rebecca;
TRAN, Lucy L.;
CEPEDA, Javier;
KONDA, Kelika Anne;
SILVA SANTISTEBAN, Alfonso;
CÁCERES PALACIOS, Carlos Fernando;
KELLY, Sherrie;
ALTICE, Frederick L.;
MARTIN, Natasha K.