Resum
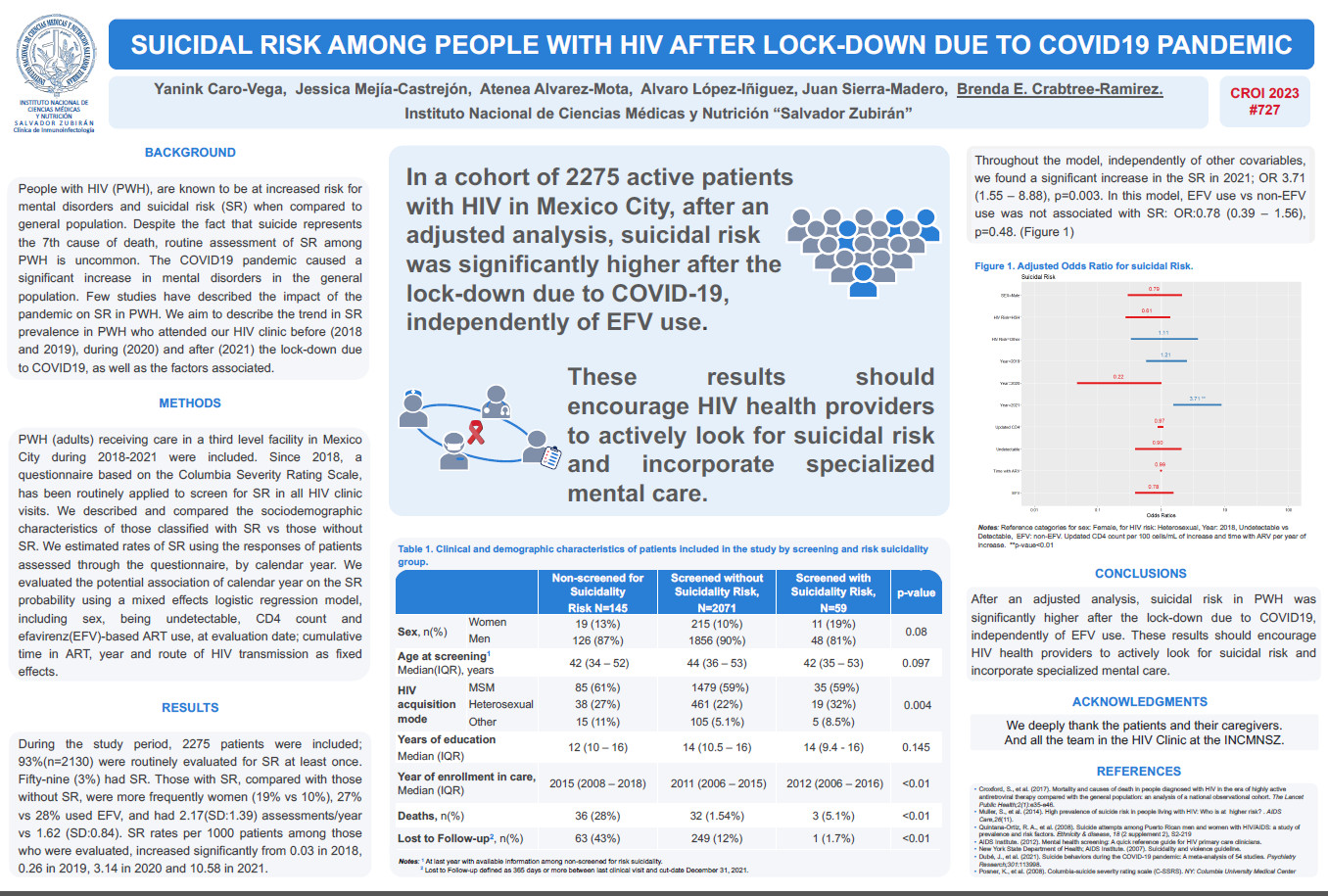
Background: People with HIV (PWH), are known to be at increased risk for mental disorders and suicidal risk (SR) when compared to general population. Despite the fact that suicide represents the 7th cause of death, routine assessment of SR among PWH is uncommon. The COVID19 pandemic caused a significant increase in mental disorders in the general population. Few studies have described the impact of the pandemic on SR in PWH. We aim to describe the trend in SR prevalence in PWH who attended our HIV clinic before (2018 and 2019), during (2020) and after (2021) the lock-down due to COVID19, as well as the factors associated. Methods: PWH (adults) receiving care in a third level facility in Mexico City during 2018-2021 were included. Since 2018, a questionnaire based on the Columbia Severity Rating Scale, has been routinely applied to screen for SR in all HIV clinic visits. We described and compared the sociodemographic characteristics of those classified with SR vs those without SR. We estimated SR using the responses of patients assessed through the questionnaire, by calendar year. We evaluated the potential association of calendar year on the SR probability using a mixed effects logistic regression model, including sex, being undetectable, CD4count and efavirenz(EFV)-based ART use, at evaluation date; cumulative time in ART, year and route of HIV transmission as fixed effects. Results: During the study period, 2275 patients were included; 93%(n=2130) were routinely evaluated for SR at least once. Fifty-nine (3%) had SR. Those with SR, compared with those without SR, were more frequently women (19%vs10%), 27% vs 28% used EFV, and had 2.17(SD:1.39) assessments/year vs 1.62 (SD:0.84). SR rates per 1000 patients among those who were evaluated, increased significantly from 0.03 in 2018, 0.26 in 2019, 3.14 in 2020 and 10.58 in 2021. Throughout the model, independently of other covariables, no significant changes in SR were observed during 2019 and 2020, compared to 2018: OR 1.21 (0.57–2.52), p=0.61 and OR 0.21 (0.05–1.00), p=0.06; but we found a significant increase in the SR in 2021; OR 3.71 (1.55–8.88), p=0.003. In this model, EFV use vs non-EFV use was not associated with SR: OR:0.78 (0.39–1.56), p=0.48. Conclusions: After an adjusted analysis, suicidal risk in PWH was significantly higher after the lock-down due to COVID19, independently of EFV use. These results should encourage HIV health providers to actively look for suicidal risk and incorporate specialized mental care.