Catálogo general VIH

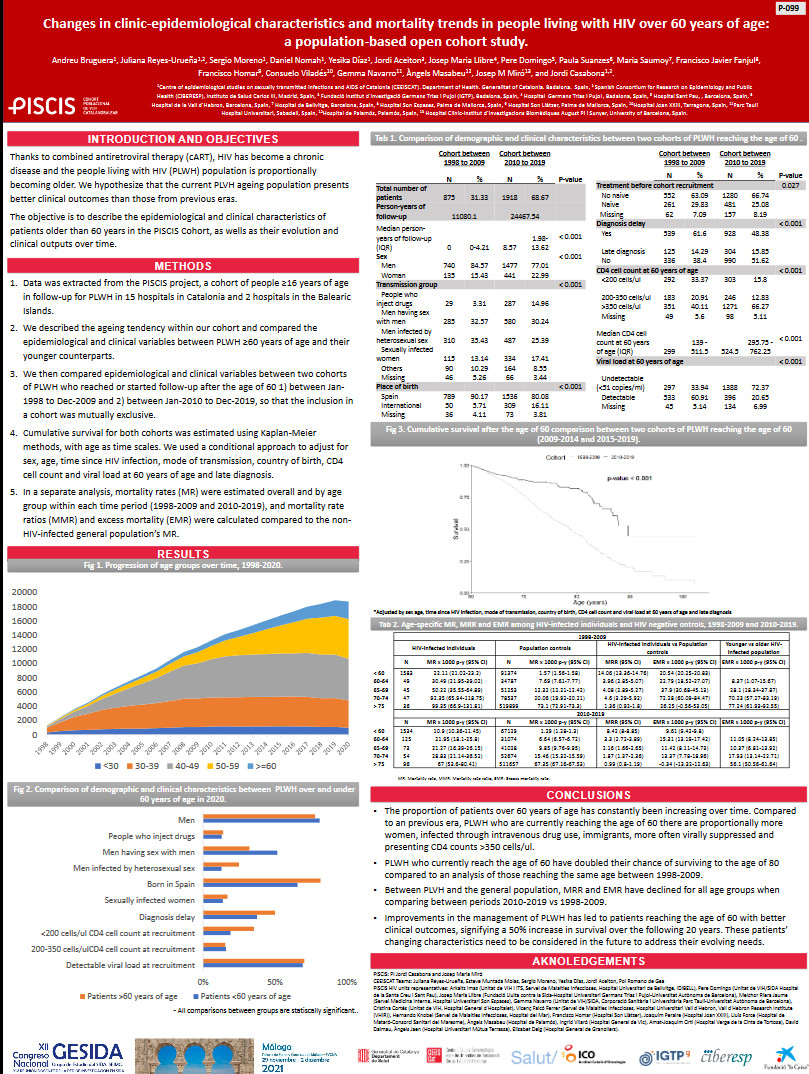
Changes in clinic-epidemiological characteristics and mortality trends in people living with HIV over 60 years of age: a population-based open cohort study.
Resumen
Background: Thanks to combined antiretroviral therapy (cART), HIV has become a chronic disease and the HIV population is proportionally becoming older. Our objective is to assess how survival has changed over time in people living with HIV (PLWH) over 60 years of age has evolved over time. Methods: Data was extracted from the PISCIS project, a cohort of people =16 years of age in follow-up for PLWH in Catalonia and Balearic Islands. We compared epidemiological and clinical variables between two cohorts of PLWH who reached or started follow-up after the age of 60 1) between Jan-1998 to Dec-2009 (C09) and 2) between Jan-2010 to Dec-2019 (C19), so no patient from C09 is included in C19. Cumulative survival for both cohorts was estimated using Kaplan-Meier methods, with age and length of infection as time scales. Mortality rates (MR) were estimated over-all and by age group within each time period (1998-2009 and 2010-2019), and mortality rate ratios (MMR) and excess mortality (EMR) were calculated compared to the general population’s MR. Results: Of the 28.120 persons recruited in PISCIS, C09 included 877 persons, and C19 1.919. Compared to cohort C09, in C19 there were higher proportions of women (15.5% vs 22.9%), people who inject drugs (PID) (3.5% vs 15.6%) and women infected via sex (13.9% vs 18%), people born outside Spain (10.7% vs 20.3%), and patients with non-delayed HIV diagnosis (34.9 % vs 46.4%) (all p<0.001). C19 had a higher proportion of patients with undetectable viral load (35.4% vs 78.8%), >350 cell/mm3 (42.4% vs 73.9%) at 60 (all p<0.001). In general, at the age of 80, C19 patients had 22% higher over-all survival than C09 patients. When taking time since infection into account, patients in C19 survived 36% more than C09 after 20 years of infection, and 50% after 30 years. By age groups, all PLWH groups had higher MR than their general population counterparts, except those >75 years of age between 2010-2019, which had similar MR (66.7 p-y [Confidence Interval (CI): 53.4-80 p-y]) to the general population (67.4 p-y [CI: 67.2-67.5 p-y]). Conclusion: In the last 10 years, in HIV patients who reach the age of 60 there are proportionally more women, PID and immigrants. They are also more often virally suppressed and present higher CD4 counts, leading to a longer life and present a lower MR than their general population counterparts.- Tema:
Autoría:
BRUGUERA RIERA, Andreu; REYES URUEÑA, Juliana; NOMAH, Daniel Kwakye; MORENO FORNES, Sergio; DÍAZ, Yesika; ACEITÓN CARDONA, Jordi; LLIBRE CODINA, Josep Maria; DOMINGO PEDROL, Pere; SUANZES, Paula; SAUMOY, María; FANJUL LOSA, Francisco Javier; HOMAR BORRÁS, Francisco; NAVARRO, Gemma; MASABEU, Àngels; MIRÓ MEDA, José María; CASABONA BARBARÀ, Jordi
Autoría institucional: Grupo de estudio PISCIS
Autoría institucional: Grupo de estudio PISCIS
Ficha bibliográfica
- Año de publicación:
- [2021]
- Descripción física:
- [1] p.
- Formato:
- Folleto
- Tipo de documento:
- Coloquios y ponencias
- Notas:
- Poster presentado en el XII Congreso Nacional de Gesida, celebrado del 29 de noviembre al 2 de diciembre de 2021 en Málaga (España).
Contenidos relacionados
También te pueden interesar
-
Impact of aging on the HIV-infected population of Catalonia and the Balearic Islands: a population-based cohort study
-
Predictors of poor health-related quality of life among people living with HIV aged =60 years in the PISCIS cohort: findings from the Vive+ project
-
Cohort Profile: PISCIS, a population-based cohort of people living with HIV in Catalonia and Balearic Islands